Introduction: Why Lower Extremity Re-Injury Rates Haven’t Budged
ACL rehab keeps advancing. Our surgical techniques are better. Our rehab progressions are more sophisticated. Our return-to-play conversations are more nuanced. However, despite all that progress, the numbers still convey the same message.
Let’s start with the data we can’t ignore.
More than 200,000 occur every year in the United States, and the re-injury numbers are sobering. Depending on the study, anywhere from 6% to over 30% of athletes will tear the same ACL again after returning to sports. That means nearly a third of some populations are repeating the same long, difficult journey.
What makes this even more concerning is that many athletes are “passing” the strength tests we traditionally rely on, yet are still returning with large deficits in reactive ability. One recent paper found that approximately 65% of patients who met their isometric strength criteria were still failing reactive strength tests. It is hard to ignore what that tells us. What we have been doing is not enough.
- Second ACL injuries remain far too common
A large cohort study found that 6 to 31 percent of athletes will suffer a second ACL injury after returning to sport, depending on age and level of competition. (Paterno et al.)
That is not a small problem. That is a system-level issue.
- Strength symmetry does not equal reactive readiness
A 2024 paper showed that roughly 65 percent of patients who passed their isometric
quadriceps strength test still failed reactive strength testing. (Girdwood et al 2024)
The authors end the study with a clear warning:
Restoring strength does not guarantee restoring reactive ability.
This is exactly where many second injuries occur, in the reactive, fast, unpredictable moments that strength tests can’t capture.
- Traditional hop tests don’t capture what we need
A study evaluating the relationship between single-leg hop performance and knee extension strength found the relationship to be moderate but imprecise, and the prediction error was clinically meaningful. (Turk 2025)
Hop distance alone cannot be used as a proxy for strength or load tolerance.
- Time alone is not protection
Other research highlights that athletes returning before nine months face dramatically higher re-injury rates. (Grindem 2016)
But even hitting the nine-month mark doesn’t guarantee that reactive qualities have returned.
Calendar time doesn’t heal the stretch-shortening cycle.
Taken together, the message is straightforward.
What we’ve been doing for return to play isn’t enough.
Too many athletes are passing strength tests or hop tests but still lack the reactive capacity, multi-planar control, and symmetry required to actually withstand sport.
This is why objective, affordable, repeatable reactive testing needs to become the standard, not the exception.
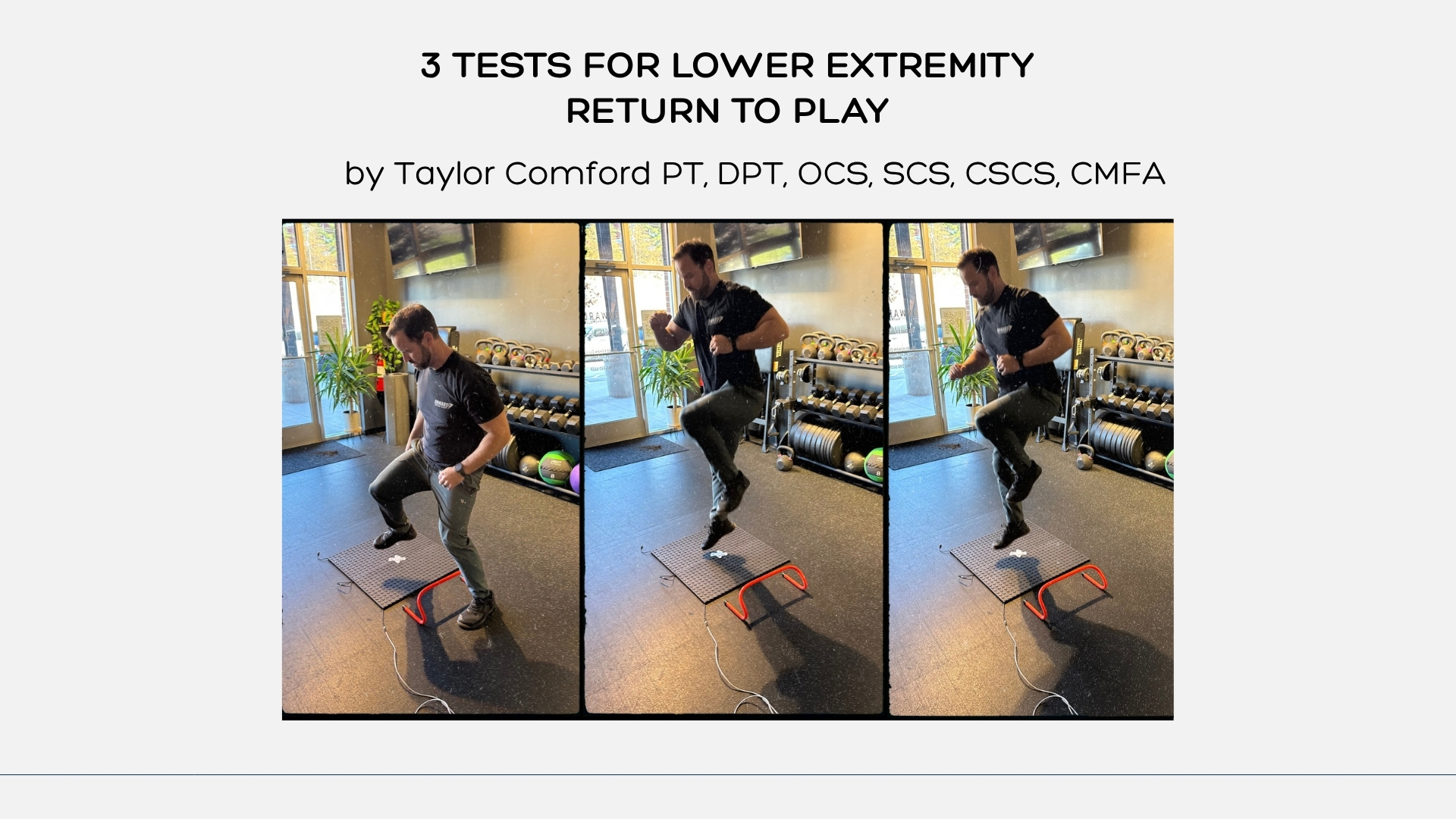
The Plyomat makes that possible without slowing a clinic down or requiring force plates. Below are the three tests I use consistently in ACL and lower-extremity rehab, each providing specific and practical information that helps guide decision-making.
1. Single Leg Vertical Jump
The single-leg vertical jump is simple, fast, and revealing. It gives you a clean look at three things.
Displacement
How much height the athlete can produce on each leg. Not just best jump, but consistency across trials with an average of 3 attempts per leg.
Control
Landing mechanics, trunk positioning, how the knee organizes under load, and whether the athlete maintains posture without wobbling or collapsing.
Competency and Confidence
This might be the most important piece. You can see exactly when an athlete is hesitant, cautious, or fearful during propulsion or landing.
How I run it
I collect three maximal attempts per side, film from the front, and compare both legs for mechanics. Athletes often spot their own compensations immediately once they see the video. <10 percent asymmetry in height is passing, but I’m evaluating all aspects, to assess the overall grade here.
This test sets the baseline for later reactive work. If an athlete cannot produce or control vertical displacement symmetrically, they are not ready to progress.
2. Single Leg 5-Hop RSI (Plotted on the RSQ)
This is the reactive strength test I rely on most, but it can also be the most intensive.
The athlete performs five consecutive maximal hops on one leg, staying tall and minimizing ground contact time. They then repeat on the other leg. The Plyomat calculates RSI from each hop, and I plot both legs on the RSQ (Reactive Strength Quadrant).
The RSQ turns the data into an immediate visual story. You see which leg has shorter contact times, which one produces better flight times, and whether both limbs fall into similar zones of reactivity. Hop distance alone does not provide the level of detail that I seek in clinical practice. You can’t make good decisions with bad data.
Clinically, the 5-Hop RSI helps uncover:
- Asymmetries masked by strength tests
- Compensation strategies that slow ground contact
- Tendon or neuromuscular limitations
- Gaps in confidence or rhythm
I hold the line at 10 percent symmetry, but that is paired with video to confirm clean, efficient movement.
This is the test where most athletes realize strength does not automatically equal reactivity. Their stronger leg is often the leg with slower contacts.
3. Lateral-to-Vertical RSI
This is the test that often determines whether I feel comfortable clearing an athlete for true sport activity. We are actively validating this test in a clinical trial with excellent reliability and reproducibility between test sites.
Most ACL injuries don’t happen in a straight vertical pattern. They happen when an athlete loads laterally, accepts force, and then tries to redirect it. The lateral-to-vertical RSI captures this exact sequence; and thus has high carryover in the discussion for return to sport for our athletes.
How the test works
The athlete starts beside the Plyomat, performs a controlled lateral bound (skater jump) over an 8” mini hurdle onto the mat, and immediately transitions into a maximal vertical jump. The distance the hurdle is from the center of the Plyomat is = Leg Length/2.
What this test reveals:
- Lateral load tolerance
- Multi-planar stiffness and control
- Timing and sequencing during force redirection
- Whether hesitation or trunk deviation appears on the involved side
It is not unusual to see an athlete test symmetrical in vertical tasks, only to show clear differences once the plane of motion changes. This test exposes that.
A limb-to-limb difference under 10 percent, paired with stable movement, is my threshold for true readiness. Oftentimes my athletes will do really well with dynamometry testing, and traditional hop testing (crossover, 3 hop for distance, 6 meter hop for time) yet still can’t pass this test.
How These Three Tests Fit Together
Here is the practical framework:
Single Leg Vertical Jump
Used in the mid to late stages. Measures displacement, control, and competency.
5-Hop RSI with RSQ Plotting
Used in late rehab and through final progression. Measures pure reactive strength and symmetry.
Lateral-to-Vertical RSI
Used for final clearance. Measures multi-planar reactivity and real sport-like force redirection.
Each test gives a different piece of the puzzle. Together they create a complete picture of lower-extremity readiness.
Affordability for Clinicians
Force plates are phenomenal tools. They give depth and detail that no clinician would deny. But they are not required to evaluate whether an athlete is reactive, symmetric, and mechanically sound.
With a high-quality contact mat and slow-motion video, you can get everything you need for return-to-play decision-making:
- Ground contact times
- Flight times
- RSI
- Multi-planar loading behavior
- Visual confirmation of movement pattern quality
The key is consistency and fast testing. The Plyomat sets up in under three minutes, and in some clinics can be installed directly into the flooring so there is no setup time at all. In a high-volume environment, this matters.
Final Thoughts After Three Years of Daily Use
After nearly three years of using the Plyomat with lower-extremity cases, I am still finding new ways it supports the process. Every ACL, meniscus repair, ankle reconstruction, and patellar tendon case teaches us something. And every retest brings clarity to what is improving, what is plateauing, and what needs more work.
The research continues to point in the same direction.
We cannot rely on strength tests alone.
We cannot assume hop distance equals readiness.
We cannot let time on the calendar guide decision-making.
We need objective measures of reactive strength, symmetry, rhythm, and multi-planar control.
These three Plyomat tests provide that structure. They are simple, fast, and repeatable. Most importantly, they give athletes the confidence that their body is ready; not just strong, but responsive, coordinated, and prepared for the instability of sport.
References
Girdwood MA, Crossley KM, Rio EK, et al. Hop to It! A Systematic Review and Longitudinal Meta-analysis of Hop Performance After ACL Reconstruction. Sports Medicine. Published online October 16, 2024. doi:https://doi.org/10.1007/s40279-024-02121-1
Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. British Journal of Sports Medicine. 2016;50(13):804-808. doi:https://doi.org/10.1136/bjsports-2016-096031
Paterno MV. Incidence and Predictors of Second Anterior Cruciate Ligament Injury After Primary Reconstruction and Return to Sport. Journal of Athletic Training. 2015;50(10):1097-1099. doi:https://doi.org/10.4085/1062-6050-50.10.07
Turck SM, Faria Silva M, Francys Vidmar M, et al. Using the Single-Leg Hop Test to Determine Knee Extension Strength After Anterior Cruciate Ligament Reconstruction. Orthopaedic Journal of Sports Medicine. 2025;13(4). doi:https://doi.org/10.1177/23259671241303520
From the Blog
Introducing the Plyomat Power Score (PPS)
When assessing Lower Body Power as mentioned in last week’s blog: Switch Mats...
Switch Mats as a Force Plate Alternative
In the world of athlete assessment, one question that continues to surface is...